Volker Vallon Research
The Vallon lab aims to integrate aspects of vascular, tubular and metabolic function to gain a more complete understanding of renal physiology, pathophysiology and pharmacology. The group has characterized the roles played by a variety of ion channels, transporters, receptors and intracellular signaling pathways in the biology of the kidney. The work offers new insights into the role of the kidney in the regulation of blood pressure, the excretion and renal clearance of exogenous and endogenous compounds, and the underlining pathophysiology of the early diabetic kidney as well as of acute kidney injury (AKI) and chronic kidney disease (CKD). The work is a blend of physiology, molecular biology and pharmacology. It uses gene-targeted mouse models to dissect contributions of specific genes and address clinically relevant questions. The group is one of few that performs in vivo renal micropuncture at the single nephron level of rodents.
Tubular Transport Mechanisms
The Vallon lab contributed to a better understanding of various renal transport mechanisms. Examples include the demonstration that TRPV5 is the gate keeper of Ca2+ reabsorption along the distal convolution and that proximal tubular hyperreabsorption explains the thiazide-induced hypocalciuria, and that dietary Na+ inhibits the open probability of the epithelial sodium channel ENaC by enhancing P2Y2 receptor tone. The group was the first to show that dietary K+ modulates the expression and phosphorylation of the Na-Cl cotransporter NCC. The Vallon lab also helped to define the role of the serum and glucocorticoid inducible kinase SGK1 in renal salt and potassium handling and in mineralocorticoid-induced salt appetite. The group also established the role of the organic anion transporter OAT1 in renal PAH secretion, OAT3 in renal creatinine and empagliflozin secretion and in the transport of an endogenous blood pressure regulator, and of both OAT1 and OAT3 in the renal secretion of loop diuretics and thiazides.
Publications:
- Vallon V, Unwin RJ, Inscho EW, Leipziger J, Kishore BK. P2 Receptors in Renal Function and Disease. Physiol Rev, 100:211-269, 2020.
- Vallon V. Glucose Transport in the Kidney in Health and Disease. Pflugers Arch, 472:1345-1370, 2020.
- Koepsell H, Vallon V. A Special Issue on Glucose Transporters in Health and Disease. Pflugers Arch, 472:1107-1109, 2020.
The Diabetic Kidney
Dr Vallon, in close collaboration with Dr Thomson, generated experimental evidence for a primary tubular hyper-reabsorption and a tubulocentric hypothesis of nephron hyperfiltration in diabetes. The work showed the critical role of sodium-dependent glucose transport (SGLT) and tubular growth for diabetic hyperfiltration. Dr Vallon discovered the salt paradox of the diabetic kidney, an unusual response of kidney growth and hyperfiltration to low dietary salt in diabetes, and showed that it is explained by the hypersensitivity of proximal tubular reabsorption to changes in dietary salt intake. The work aims to develop a unifying hypothesis that links early changes in the diabetic kidney to progressive kidney disease, putting the tubular growth response and its molecular signature at the very center.
Publications:
- Vallon V, Thomson SC. The Tubular Hypothesis of Nephron Filtration and Diabetic Kidney Disease. Nature Rev Nephrol, 16:317-336, 2020.
- Vallon V, Thomson S. Renal function in diabetic disease models: The tubular system in the pathophysiology of the diabetic kidney. Annu Rev Physiol, 74:351-375, 2012.
- Vallon V. The proximal tubule in the pathophysiology of the diabetic kidney. Am J Physiol Regul Integr Comp Physiol. 300:R1009-22, 2011.
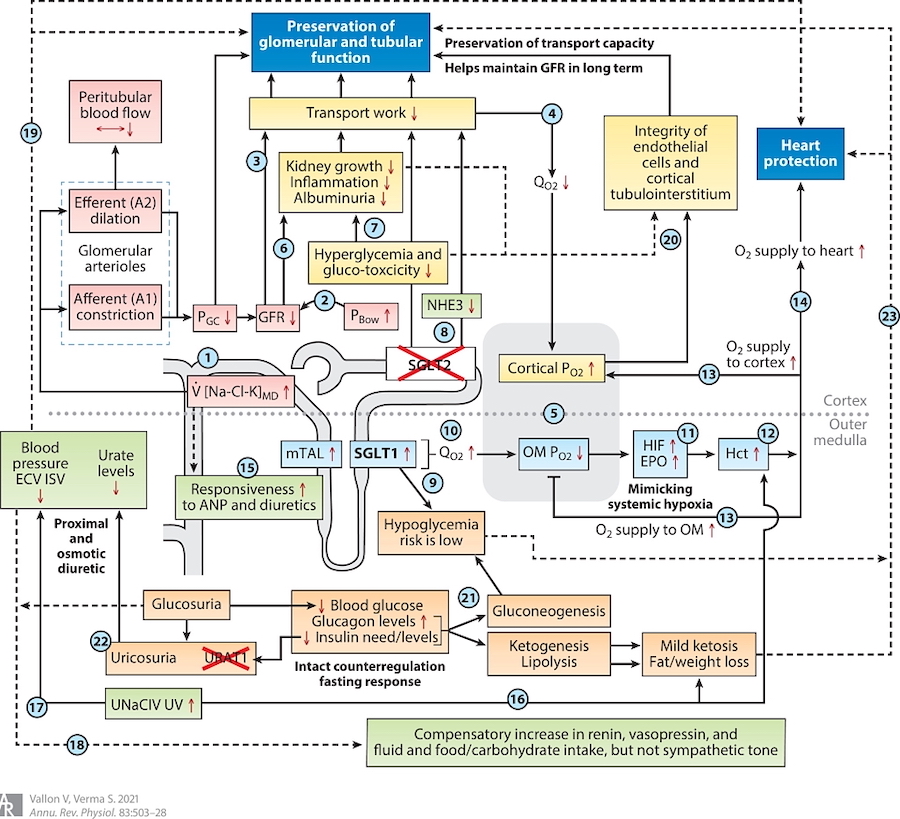
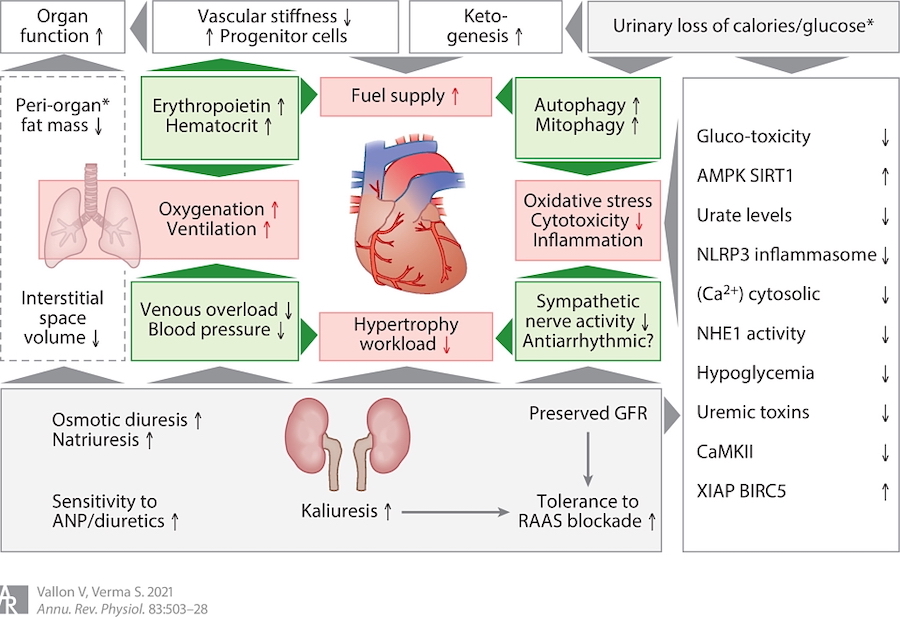
Sodium Glucose Cotransport
The Vallon lab performed critical experimental studies to established the basic physiology and pathophysiology of the sodium-glucose cotransporter SGLT2 in the normal and diabetic kidney.
Publications:
- Vallon V. Mechanisms of action of SGLT2 inhibitors and clinical implications. Am J Hypertension, 37:841-852, 2024. https://academic.oup.com/ajh/article/37/11/841/7715783?utm_source=authortollfreelink&utm_campaign=ajh&utm_medium=email&guestAccessKey=17fb2879-dd8d-49b5-aede-e25b846c8d25
- Vallon V, Nakagawa T. Renal tubular handling of glucose and fructose in health and disease. Compr Physiology, 29;12:2995-3044, 2022.
- Vallon V, Verma S. Effects of SGLT2 Inhibitors on Kidney and Cardiovascular Function. Annu Rev Physiol, 83:503-528, 2021.
- Thomson SC, Vallon V. Renal Effects of Sodium-Glucose Co-Transporter Inhibitors. Co-Published in American Journal of Medicine, 132:S30-S38, 2019 & AM J Cardiol, 124:S28-S35, 2019.
- Qiu H, Novikov A, Vallon V. Ketosis and diabetic ketoacidosis in response to SGLT2 inhibition: basic mechanisms and therapeutic perspectives. Diabetes/Metabolism Research and Reviews, Jul;33(5). doi: 10.1002/dmrr.2886, 2017.
- Nespoux J, Vallon V. SGLT2 inhibition and kidney protection. Clin Sci (Lond) 132:1329-1339, 2018.
- Layton AT, Vallon V. Renal tubular solute transport and oxygen consumption: insights from computational models. Curr Opin Nephrol Hypertens 27:384-389, 2018.
- Vallon V, Thomson SC. Targeting renal glucose reabsorption to treat hyperglycaemia: the pleiotropic effects of SGLT2 inhibition. Diabetologia, 60:215-225, 2017.
- Vallon V. The mechanisms and therapeutic potential of SGLT2 inhibitors in diabetes mellitus. Annu Rev Med, 66:255-70, 2015.
- Gallo L, Wright EM, Vallon V. Probing SGLT2 as a therapeutic target for diabetes: basic physiology and consequences. Diab Vasc Dis Res, 12:78-89, 2015.
The Pleiotropic Effects of SGLT2 Inhibition on Kidney and Heart
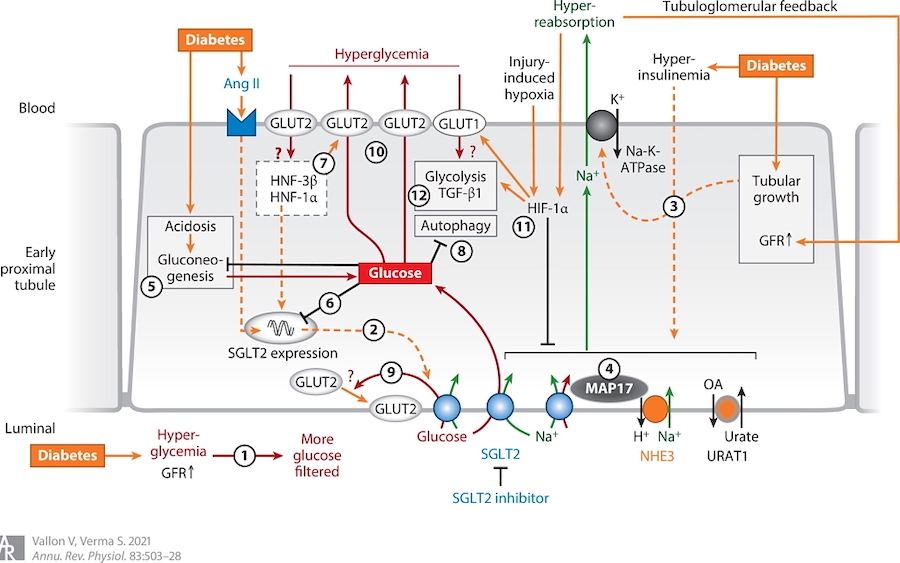
Figure 1. Pleiotropic Effects of SGLT2 Inhibition on Kidney and Heart — Scheme 1
Ongoing Work
The current work of the Vallon lab is focusing on the functional and physical interaction of SGLT2 with other transporters in the early proximal tubule (incl. URAT1, NHE3), the consequences of SGLT2 inhibition on these transporters as well as on the metabolic and gene and protein expression profile ("inner workings") of the early versus late proximal tubule, the off-target effect of SGLT2 inhibitors on the microbiome formation of uremic toxins, as well as new strategies to target metabolic and kidney disease, including the role of the early proximal tubule amino acid transporter SLC6A19 and of SGLT1 as a glucose sensor in the macula densa.
- Kim YC, Das V, Kanoo S, Yao H, Stanford SM, Bottini N, Karihaloo A, Vallon V. Transcriptomics of SGLT2-positive early proximal tubule segments in mice: response to type 1 diabetes, SGLT1/2 inhibition or GLP1 receptor agonism. Am J Physiol Renal Physiol, 328(1):F68-F81, 2025.
- Oe Y, Kim YC, Kanoo S, Goodluck HA, Lopez N, Diedrich J, Pinto AM, Evensen KG, Currais A, Maher P, Vallon V. Western diet exacerbates a murine model of Balkan nephropathy. Am J Physiol Renal Physiol, 328(1):F15-F28, 2025.
- Billing A, Kim YC, Gullaksen S, Schrage B, Raabe J, Hutzfeldt A, Demir F, Kovalenko E, Lasse M, Dugourd A, Fallegger R, Klampe B, Jaegers J, Li Q, Kravtsova O, Crespo-Masip M, Palermo A, Hoxha E, Fenton R, Blankenberg S, Kirchhof P, Huber T, Laugesen E, Zeller T, Chrysopolou M, Saez-Rodriguez J, Magnussen C, Eschenhagen T, Staruschenko A, Siuzdak G, Poulsen PL, Schwab C, Cuello F, Vallon V*, and Rinschen M*; * shared senior authorship. Metabolic communication by SGLT2 inhibition. Circulation, 149:860–884, 2024.
- Oe Y, Kim YC, Sidorenko VS, Zhang H, Kanoo S, Lopez N, Goodluck HA, Crespo Masip M, Vallon V. SGLT2 inhibitor dapagliflozin protects the kidney in a murine model of Balkan nephropathy. Am J Physiol Renal Physiol, 326:F227-F240, 2024.
- Kim YC, Fattah HM, Fu Y, Nespoux J, Vallon V. Expression of leptin receptor in renal tubules is sparse but implicated in leptin-dependent kidney gene expression and function. Am J Physiol Renal Physiol, 324:F544-F557, 2023.
- Zhang J, Cai J, Cui Y, Jiang S, Wei J, Kim YC, Chan J, Thalakola A, Le T, Xu L, Wang L, Jiang K, Wang X, Wang H, Cheng F, Buggs J, Koepsell H, Vallon V, Liu R. Role of the macula densa sodium glucose cotransporter type 1-nitric oxide synthase 1-tubuloglomerular feedback pathway in diabetic hyperfiltration. Kidney Int. 101(3):541-550, 2022.
- Navarro-Garrido A, Kim YC, Oe Y, Zhang H, Crespo-Masip N, Goodluck HA, Kanoo S, Sanders PW, Broer S, Vallon V. Aristolochic acid-induced nephropathy is attenuated in mice lacking the neutral amino acid transporter B0AT1 (Slc6a19). Am J Physiol Renal Physiol, 323(4):F455-F467, 2022.
- Thomson SC, Vallon V. Effects of SGLT2 inhibitor and dietary NaCl on glomerular hemodynamics assessed by micropuncture in diabetic rats. Am J Physiol Renal Physiol, 320:F761-F771, 2021.
- Onishi A, Fu Y, Patel R, Darshi M, Crespo-Masip M, Huang W, Song P, Freeman B, Kim YC, Soleimani M, Sharma K, Thomson SC, and Vallon V. A role for the tubular Na+-H+-exchanger NHE3 in the natriuretic effect of the SGLT2 inhibitor empagliflozin. Am J Physiol Renal Physiol, 319:F712-F728, 2020.
- Song P, Huang W, Onishi A, Patel R, Kim Y, van Ginkel C, Fu Y, Freeman B, Koepsell H, Thomson SC, Liu R, Vallon V. Knockout of Na-Glucose-Cotransporter SGLT1 Mitigates Diabetes-Induced Upregulation of Nitric Oxide Synthase-1 in Macula Densa and Glomerular Hyperfiltration. Am J Physiol Renal Physiol. 317:F207-F217, 2019.
- Novikov A, Fu Y, Huang W, Freeman B, Patel R, van Ginkel C, Koepsell H, Busslinger M, Onishi A, Nespoux J, Vallon V. SGLT2 inhibition and renal urate excretion: the role of luminal glucose, GLUT9 and URAT1. Am J Physiol Renal Physiol 316:F173-F185, 2019.
- Zhang J, Wei J, Jiang S, Xu L, Wang L, Cheng F, Buggs J, Koepsell H, Vallon V, Liu R. Macula Densa SGLT1-NOS1-TGF Pathway - A New Mechanism for Glomerular Hyperfiltration During Hyperglycemia. J Am Soc Nephrol, 30:578-593, 2019.
- Layton AT, Vallon V. SGLT2 inhibition in a kidney with reduced nephron number: modeling and analysis of solute transport and metabolism. Am J Physiol Renal Physiol, 314:F969-F984, 2018.
